Official The AFIB Clinic Blog

Afib Ablation
Afib Medications
Atrial Fibrillation
Caffeine
clinical trials
Exercise
Introductory
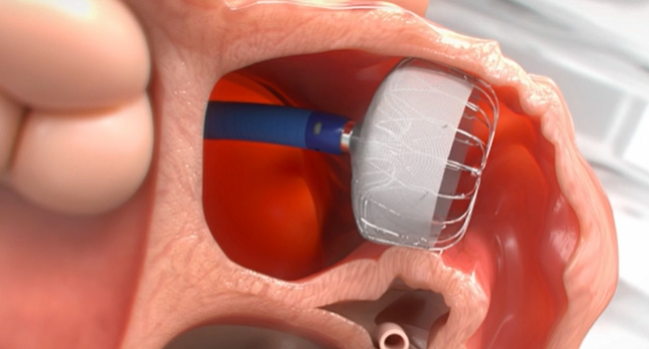
left atrial appendage
Patient Testimonials
Physician Resources
Pulsed Field Ablation
research
watchman
Wearables - Apple Watch