Dr Jose Osorio performing an Afib ablation
Treatment Options for Atrial Fibrillation (AFib)
Atrial fibrillation is the most common sustained cardiac arrhythmia. The number of patients with AFib continues to grow but fortunately, so do the treatment options. You have learned in our previous sections about what AFib is and the consequences it may have. We will now focus on the treatment options available for patients with AFib.
In treating someone with atrial fibrillation it is important to always focus on the three main problems it may cause:
- Strokes: AFib increases the stroke risk fivefold.
- Symptoms: AFib may cause a variety of symptoms and can
decrease your quality of life - Congestive heart failure: If not treated properly afib may cause congestive heart failure in some patients
The treatment for atrial fibrillation is always individualized, tailored to a patient’s needs, risk factors for stroke and congestive heart failure, and most importantly how much AFib has affected your quality of life. The treatment is also dependent upon whether a patient has paroxysmal, persistent, or permanent atrial fibrillation.
In treating a patient with AFib, I always like to follow a step-wise approach.
Step 1: Stroke Prevention
Determine the patient’s stroke risk and based on that choose the most appropriate stroke prevention option.
Every patient with AFib has an increased risk of having a stroke. Strokes happen when blood clots form inside the left atrium and if dislodged travel to the brain where they can cut off circulation.
Your risk of stroke is dependent upon what other risk factors you have. The appropriate treatment to decrease your risk of stroke will be dependent on how high your risk is. Your physician will also take into consideration along with you how high your risk of bleeding from blood thinners is.
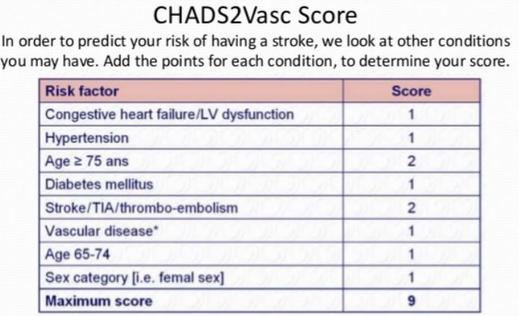
CHADS2Vasc score is used to evaluate the risk stroke for patients with Atrial Fibrillation. Add points based on each condition the patient has and then use the table below to see your yearly risk of stroke
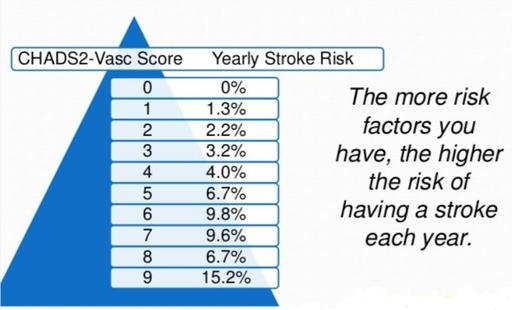
CHADS2Vasc score is used to evaluate the risk stroke for patients with Atrial Fibrillation. The more risk factors a patient has, the higher the risk
Low Stroke risk patients: for many patients with Afib, blood thinners may not be indicated. The risk of stroke is low and therefore a blood thinner may offer more risks than benefits.
Moderate or high risk patients: blood thinners (such as coumadin, dabigatran, apixaban, or rivaroxaban) are indicated for patients with Afib and that have many risk factors. Some patients are unable to take oral anti-coagulant medications long term and left atrial appendage closure (watchman device) may be an alternative.
AFib, Stroke, and Bleeding Risk
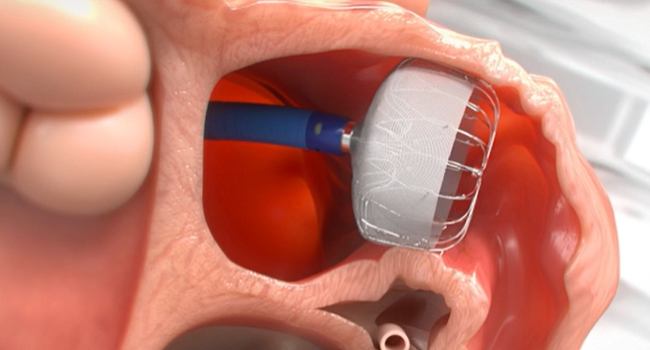
Left Atrial Appendage Closure using the Watchman FLX device
Stroke reduction with either blood thinners or left atrial appendage closure is indicated for most patients with AFib. Some patients are unable to take blood thinners due to a high bleeding risk. Left atrial appendage closure is a good alternative for these patients.
AFib treatment is always individualized and should be carefully discussed with your physician. Please see more details about stroke prevention in our section about stroke. Always remember that this booklet is supposed to be informational only and that treatment is individualized and should be discussed with your physician.
Step 2: Improve Quality of Life – Reducing the symptoms caused by Afib
 Determine how symptomatic a patient is and based on that determine if rate or rhythm control is the most appropriate option.
Determine how symptomatic a patient is and based on that determine if rate or rhythm control is the most appropriate option.
Patients with atrial fibrillation can be extremely symptomatic while some have no symptoms at all. Some patients have few spells a year, while others have many spells a week. Others are in AFib all the time. These are the factors that will determine the treatment. There are different types of atrial fibrillation, and the treatment may differ depending on the type the patient has.
Patients With Paroxysmal AFib
Spells that stop spontaneously, typically lasting less than 24 hours. Depending on the number and severity of the spells the treatment will consist of:
- Beta blockers or calcium channel blockers: medications that are used to slow down your heart during spells of AFib.
- Anti-arrhythmic drugs: if a patient continues to have symptomatic spells frequently, these drugs are indicated to decrease the number of spells. When these drugs are used we call it a rhythm control strategy. There are many anti-arrhythmic drugs available. Oftentimes treatment by a physician specialized in treating rhythm disorders is necessary.
- Atrial fibrillation ablation: AFib ablation is the best option for patients who have failed or have not tolerated medications. AFib ablation is the only treatment option for patients with AFib that is potentially curative. We have an entire section dedicated to atrial fibrillation ablation.
Atrial Fibrillation ablations are performed in the Electrophysiology Laboratory. Although traditionally performed using Xray to guide the ablation, we now have tools that can guide us and most procedures can be performed with minimal or no X-ray exposure at all by experienced physicians.
Patients With Persistent AFib
Patients who stay in AFib constantly have to be treated to return to normal rhythm. In patients with persistent atrial fibrillation, the first step is to decide what is the most appropriate treatment options, rate, or rhythm control.
Rhythm control is the right option for you if you have symptoms believed to be secondary to AFib, such as fatigue, shortness of breath, dizziness, etc. Most patients are able to tell right away when they went into AFib and for these patients, it is relatively easy to decide the treatment of choice.
- Cardioversion plus anti-arrhythmic drugs: for patients with persistent atrial fibrillation to return to normal rhythm, we typically need to perform a cardioversion. A procedure where the patient is sedated for a brief period of time and then a shock is delivered to stop the AFib. After that medications have to be used to keep the patient in normal rhythm.
- AFib ablation: ablation can also be performed for patients with persistent atrial fibrillation.
Rate control is the best option for patients who are asymptomatic or just mildly symptomatic. For these patients, the treatment consists of using medications to control the heart rate. It is always important to remember that treatment to reduce the risk of stroke concurrently is necessary.
Step 3: Prevention of Congestive Heart Failure
Atrial fibrillation frequently causes increased heart rates. If the pulse rate remains elevated for a prolonged period of time (weeks or months) this can cause the heart to become week, a condition called Congestive Heart Failure.
For patients who stay in AFib, it is very important to make sure that the heart rates are well controlled at all times, both at rest and during exertion. Some patients have such fast heart rates during AFib that with time the heart can become weak – and develop congestive heart failure. It is always one of the goals of our therapy to prevent Congestive Heart Failure.
Procedures to Treat Atrial Fibrillation
Cardioversion plus Rhythm Control Medicine: For patients with persistent AFib, cardioversion may be needed to restore the heart back to a normal rhythm. This procedure is done in the EP and Cath Lab. A short-acting anesthetic is given and one or more shocks are delivered in an attempt to restore the normal heart rhythm. Afterward, rhythm control medications are used to attempt to maintain a normal rhythm.
Atrial Fibrillation Ablation: AFib ablation is the option of choice for many patients with Afib. Afib ablation technology, safety and success rates have continued to improve over the past 2 decades. Therefore, Afib ablation has become an ever more important choice and for many patients it is considered the primary treatment. Learn more about AFib Ablation >>
-
Radio Frequency Ablation Of The Pulmonary Veins:
An ablation catheter is positioned at the mouth of the pulmonary vein and ablation is performed by heating the tissue. Ablation is guided by a “Mapping system.” -
Cryoballoon Ablation Of The Pulmonary Vein:
The Cryoballoon is positioned at the pulmonary vein and ablation is performed by getting the tissue around the vein down to very cold temperatures. -
Pulsed Field Ablation:
or PFA is a new energy modality for the ablation of cardiac tissue. This technology has been approved in Europe and is undergoing clinical trials in the US.
Pacemaker: Some of the medicines used to treat AFib can make the heart beat too slowly. When this happens, a pacemaker may be implanted. The pacemaker restores a normal heart rate but it does not treat AFib.
Maze Procedure: MAZE is a surgical treatment for AFib. It is most commonly used with patients who have AFib and need heart surgery for another reason, such as bypass or valve repair surgery.
AV Node Ablation: Another option for patients is AV node ablation with the implantation of a pacemaker. This option is used when patients are not candidates for an AFib ablation and medications have been ineffective or poorly tolerated. An AV node ablation is often performed when it is not possible to maintain a normal rhythm. After the ablation, you will depend on the pacemaker to maintain your heart beats.
Dr Jose Osorio
Miami, FL
Read More About AFib: